Hemophilia Treatment
Hemophilia (type A and B) is a hereditary bleeding disorder in which the blood’s ability to clot is compromised. The disease is characterized by low levels of Factor VIII or Factor IX in the blood, which is often treated by regular intravenous (IV) infusions of replacement factor.
Typical prophylaxis regimens involve over 150 self-infusions per year, which can be extremely time-intensive depending on the patient’s treatment. As a result, for the estimated 400,000 affected patients worldwide, increasing the efficiency and convenience of intravenous self-infusion procedures could be life-altering.
Intravenous infusions administered by the patient him/herself have human factors considerations. Specifically, hemophiliacs often must administer their infusions in variable conditions. While the majority of infusions occur in the controlled, in-home environment, patients must also self-infuse in the workplace, in public, or while commuting. Lighting, stability, privacy, and cleanliness are just a few of the variables hemophiliacs must consider.
Human Factors Research to Identify Challenges
Research Collective conducted a small study to investigate the nature of the intravenous self-infusion of hemophilia medication. The goal of the study was two-fold: 1) to identify, document, and understand the challenges involved in performing IV self-infusions; and 2) to explore, compare, and contrast appropriate research methods for understanding the IV self-infusion process.
Results of the study were briefly summarized in a poster Research Collective created for the 2019 Human Factors and Ergonomics Society Healthcare Symposium. If you would like to download the poster, simply click the button below. If there are questions about the study or you would like to discuss what you read, you can contact Anders Orn.
Information from the poster is detailed below:
Background
Hemophilia (type A and B) is a hereditary bleeding disorder in which the blood’s ability to clot is compromised (Peyvandi, et al., 2016). For many, the primary means of treatment depends on the delivery of a coagulation factor medication through intravenous (IV) infusion (Srivastava, et al., 2013). On average, hemophilia patients perform self-infusions about 150 times per year — that is, about once every 2 – 3 days. What’s more, infusions can take anywhere from 2 to 50 minutes to complete (Saxena, 2013), depending on the prophylaxis treatment.
Due, in part, to the frequency and cost associated with these infusions, the vast majority of hemophiliacs perform infusions themselves. Unsurprisingly, self-administration of prophylaxis regimens introduces a number of complexities and constraints, which raise human factors concerns. To date, however, little empirical focus has been directed toward understanding the self-infusion process for those with hemophilia.
Goals
The purpose of this study was to observe people with hemophilia performing IV self-infusions using a multi-method approach. The goal was two-fold: 1) to identify, document, and understand challenges involved in performing IV self-infusions; and 2) to explore, compare, and contrast appropriate research methods for understanding the IV self-infusion process.
Method
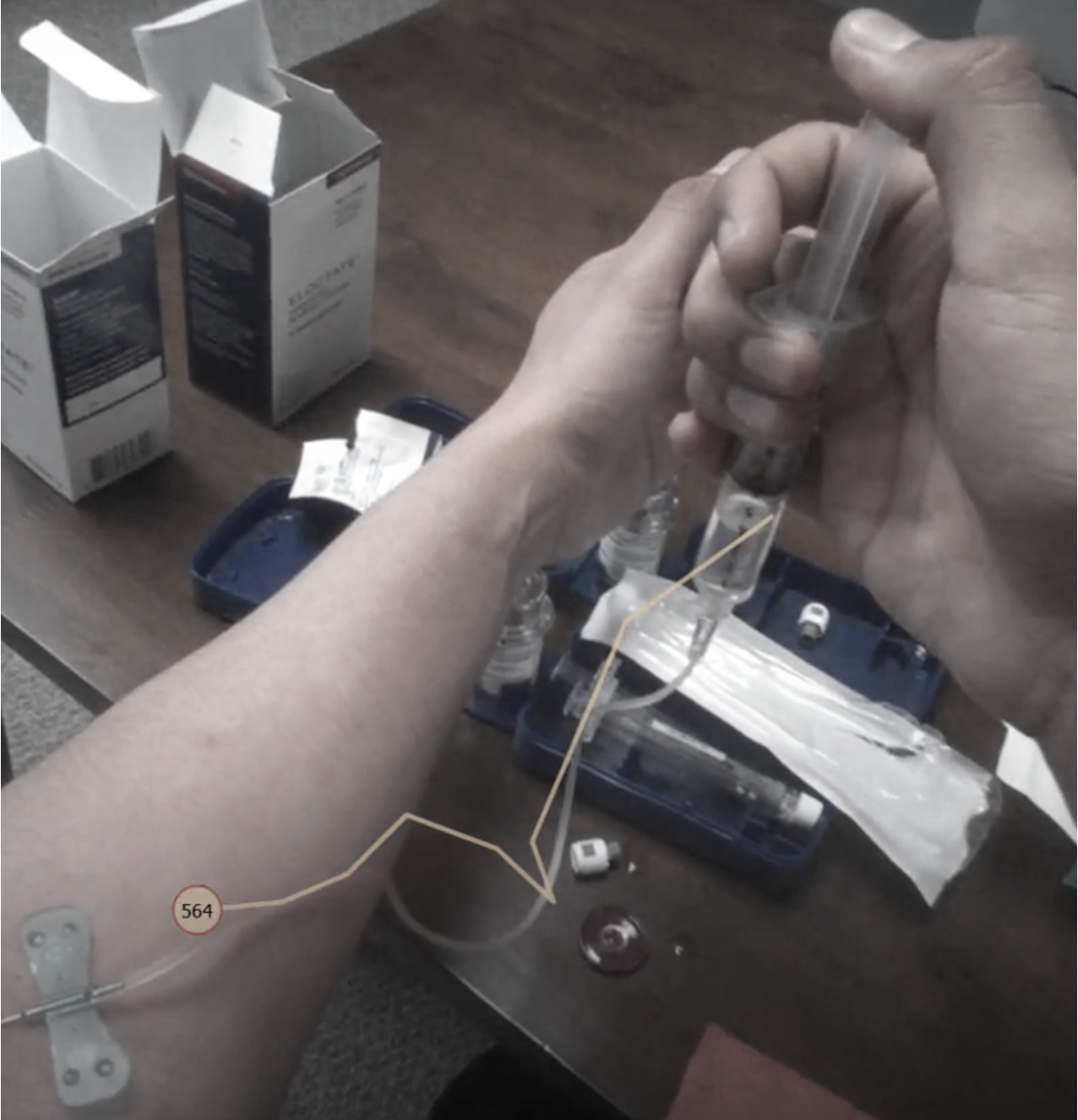
Six (6) males diagnosed with Hemophilia (type A or B) participated in this study. All participants regularly perform IV self-infusions and were at least 18 years of age. Participant ages ranged from 19 to 62 years old, with a mean of 32.7 years. While wearing eye-tracking glasses (Tobii Eye Glasses 2), participants performed a routine self-infusion at a usability lab in Tempe, AZ. Two researchers observed each self-infusion, noting time-on-task as well as the sub-steps completed. Afterwards, participants completed a semi-structured interview to explore the strengths and limitations of their current self-infusion process.
Results and Discussion
A multi-method approach was used to divide the self-infusion process into six (6) primary steps. The process is both step and time intensive, taking an average of 54 substeps over an average period of 8 minutes, 17 seconds. Based on qualitative feedback, the most difficult step in the self-infusion procedure is venipuncture. “Hitting the vein” can be frustrating, painful, and wasteful in cases where the medication does not successfully enter the vein (i.e., “blow the vein”).
Users wanted a less invasive and less complicated medication delivery method. Fixation duration, fixation frequency, and pupil size were tracked across self-infusion steps. Increased fixation duration during venipuncture and infusion suggest higher cognitive and attentional load overall. Meanwhile, fixation frequency rates were highest in material preparation steps, which may be simply due to more stimuli in the user’s field of view. Prior research suggests pupil size is positively correlated with high arousal and cognitive demands.
One a priori assumption for this study was that venipuncture steps would elicit high arousal states. Surprisingly, however, this study found that pupil size was smallest during these steps. One potential explanation is that venipuncture involves both visual and haptic feedback (i.e., the feel of the needle in the vein), thereby reducing demand on one’s visual system. Future studies are advised to test this assumption with a larger sample size.
Conclusion
This study identified six (6) general steps during self-infusion, which consist of many time consuming sub-steps. The conclusion is substantiated by user feedback. Efforts should be made by manufacturers to shorten, remove, and combine the steps required to self-infuse hemophilia medication. Hemophiliacs would also support non-IV medication delivery, should it be made possible. The multi-method approach of direct observation, task analysis, semi-structured interviewing, and eye tracking offered a unique synthesis of the self-infusion process. Eye tracking provided a quantitative approach to evaluating potential cognitive demands, beyond what is feasible through existing qualitative methods (e.g., participant self-report).
References
Peyvandi, F., Mannucci, P. M., Garagiola, I., El-Beshlawy, A., Elalfy, M., Ramanan, V., … & Manglani, M. V. (2016). A randomized trial of factor VIII and neutralizing antibodies in hemophilia A. New England Journal of Medicine, 374, 2054-2064.
Saxena, K. (2013). Barriers and perceived limitations to early treatment of hemophilia. Journal of Blood Medicine, 4, 49-56.
Srivastava, A., Brewer, A. K., Mauser‐Bunschoten, E. P., Key, N. S., Kitchen, S., Llinas, A., & Street, A. (2013). Guidelines for the management of hemophilia. Haemophilia, 19, e1-e47



